Moffitt delving into the other side of HPV
A group of girls skip rope and sing, “One less, one less, I wanna be one less” in a television commercial. Other girls stand next to road signs bearing the number one, holding signs reading “less.” Their cryptic catchphrase soon gives way to information about Gardasil – a vaccine that helps protect young women from getting cervical cancer as a result of Human Papillomavirus, or HPV.
Discussions of HPV have intensified over the past year, and while most planning has centered on its effects on young women, many advertisements – such as those made by Gardasil – touch less on the potential health effects to males.
USF is leading the way in discovering how HPV affects males through a four-year, $8-million study titled Natural History of HPV Infection in Men Study: H.I.M. The study is being administered by the HPV Research Clinic at Moffitt Cancer Center and is funded by the National Institute of Health (NIH).
Founded at Moffitt Cancer Center in the fall of 2004, the HPV Research Clinic is currently operating four different HPV research studies, all under the direction of the clinic’s project director, Martha Abrahamsen.
“Little is known regarding the prevalence, incidence and clearance of HPV infections in men, hampering efforts to control infection in both men and women,” said Abrahamsen. “The goal of this research study is to further our understanding of the natural history of HPV infection in men so that effective programs can be developed to reduce (the) HPV cancer burden in both men and women.”
Moffitt Cancer Center is collaborating with the Instituto Nacional de Salud Publica (Institute of Public Health) in Cuernavaca, Mexico, and The Ludwig Institute for Cancer Research in Sao Paulo, Brazil. Abrahamsen said the study is the largest of its kind.
“We have established research clinics in Mexico and Brazil and are recruiting men at those sites,” Abrahamsen said. “Our goal is to follow 3,000 men for four years: 1,000 men here in Tampa, 1,000 in Mexico and 1,000 in Brazil.”
Emily Jolles, clinical trials coordinator for the H.I.M study, explained the choice of those two sites.
“In general, Brazil and Mexico have higher rates of cervical cancer and dysplasia,” Jolles said. “However, rates in most Latin American and Caribbean countries are higher than 20 cases per 100,000.”
According to a Pan American Health Organization report, the number of new cases and mortality rates from cervical cancer – the world’s largest killer of women – has declined to below 10 per 100,000 females in both Canada and the United States.
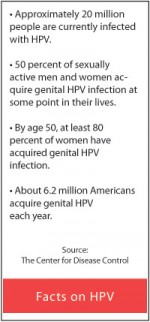
By age 50, at least 80 percent of women will have acquired genital HPV infection and approximately 20 million people are currently infected with HPV, according to the Centers for Disease Control (CDC). At least 50 percent of sexually active men and women acquire genital HPV infection at some point in their lives. According to Abrahamsen, understanding HPV in men will benefit women’s health as well.
“Research previously conducted by our group and others suggest that the sexual behavior of the male partner may be as or more important than a woman’s personal sexual behavior in predicting her risk of HPV infection and cervical disease,” Abrahamsen said. “It is important, therefore, to understand the natural history of HPV infection in men.”
Abrahamsen wants every male student at USF to know the health risks associated with HPV. It’s the most common sexually transmitted infection in men and women. In fact, at least 50-70 percent of sexually active people will have genital HPV at some point in their lives. She also said condoms do not always protect against HPV and that the infection can lead to genital warts and cancer in men and women. Most people with HPV have no signs of infection.
Perhaps the most striking fact about HPV is how it is spread. Genital HPV is spread through skin-to-skin contact, not through an exchange of bodily fluids.
There has been widespread controversy over the idea of making school entry requirements for Gardasil, the HPV vaccine. USF’s Student Health Services offers the series of three Gardasil shots for $125 to female students. While Abrahamsen cannot speak for Moffitt Cancer Center, she personally supports it.
“I support a school entry requirement for the HPV vaccine,” Abrahamsen said. “This is a known public health mechanism to ensure dissemination of vaccines. This will ensure that also high-risk people get the HPV vaccine – not only people that initiate a contact to get the vaccine. Under and un-insured children will be covered under the Vaccine for Children Program. I think the main controversy is due to people not being educated on what HPV is and what it can cause.”
Not everyone shares that position. Chinoyerem Onwunli, a USF Public Health graduate student majoring in health policy, opposes the vaccine for different reasons. “HPV is so common and researchers are not quite sure which strains cause the cancer – the likelihood of the virus causing cancer is so small,” Onwunli said. “I believe that it’s marketed toward fear. Having people get so scared and worried about it almost pressures government into having something mass produced.”
Abrahamsen said the HPV Research Clinic is still looking for healthy men ages 18-70 to participate in this study.
“It is a great opportunity to take part in a groundbreaking research study,” Abrahamsen said. “Participants will be tested and educated on HPV and other sexually transmitted infections. In addition, they will receive free health check ups and even get paid to take part in the study.”





